Rhinology Questions
August 9th, 2023
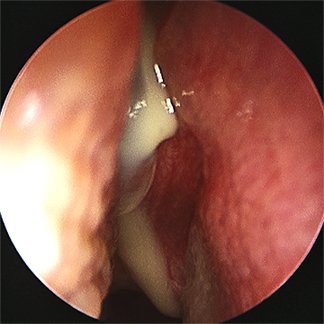
A 57-year-old-woman presents to the clinic with facial pain, nasal congestion, and nasal drainage over the past 4 days. She denies rhinorrhea, cough, or sore throat. She also states she has been unable to smell over the past 24 hours. She has never experienced these symptoms before, and she has had reliable follow-up in the past. Her temperature is 37.9ºC, heart rate is 75 bpm, blood pressure is 128/84, and respiratory rate is 16/min. Physical exam reveals tenderness to palpation over the frontal sinuses. Endoscopic exam shows bilateral nasal mucosal edema and purulent nasal secretions, as shown in the Figure. What is the next best step in management?
A) CT scan of the head
B) MRI of the head
C) Systemic glucocorticoids
D) Systemic antifungal therapy
E) Symptomatic care with 1 week follow-up
-
Correct Answer: E
Explanation:
This patient’s symptoms are suggestive of acute rhinosinusitis, which may be bacterial or viral, and requires the presence of symptoms for <4 weeks. Because a substantial number of patients with clinically diagnosed acute rhinosinusitis improve with supportive care alone, symptomatic care is generally recommended with observation for patients who can reliably return for follow-up, though initial antibiotic therapy may also be used. Systemic glucocorticoids and antifungal therapy are not indicated in the treatment of acute rhinosinusitis. Imaging should not be obtained for patients with uncomplicated acute rhinosinusitis, unless a complication or alternative diagnosis is suspected.
References:
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1-S39. doi:10.1177/0194599815572097
Image Credit: UpToDate - Acute sinusitis and rhinosinusitis in adults clinical manifestations and diagnosis [Article Link]
June 28, 2023
A 55-year-old female patient with a known history of poorly controlled diabetes mellitus presents with persistent headache, nasal congestion, and facial pain for the past two months. On examination, you note necrotic black eschar in the nasal cavity. Nasal endoscopy reveals deviated nasal septum and pale, edematous mucosa with black discoloration. Non-contrast CT sinus findings include hypoattenuated mucosal thickening in the nasal cavity with local bony erosion. Based on these findings, which of the following is the most appropriate management approach for this patient?
A) Topical corticosteroids and nasal saline irrigation
B) Oral antihistamines and intranasal corticosteroids
C) Surgical debridement and systemic antifungal therapy
D) Oral antibiotics and antipyretics
E) Observation and reassurance
-
Correct Answer: C
Explanation: The clinical presentation of necrotic black eschar, pale and edematous mucosa with black discoloration, along with a history of poorly controlled diabetes, raises suspicion for invasive fungal sinusitis. This condition is a potentially life-threatening infection characterized by invasive fungal growth within the sinuses and surrounding structures. Immediate management of invasive fungal sinusitis involves a combination of surgical debridement and systemic antifungal therapy. Surgical debridement aims to remove necrotic tissue and fungal elements from the affected sinuses, thereby reducing the fungal burden and improving the efficacy of antifungal treatment. It also helps to restore sinus drainage and facilitate the delivery of antifungal agents. Systemic antifungal therapy is essential to treat the underlying fungal infection. Agents such as amphotericin B or voriconazole are commonly used for invasive fungal sinusitis, with the choice depending on the specific fungal species involved and patient factors.
Options A and B are more appropriate for conditions like allergic rhinitis or nasal polyps, which are characterized by chronic inflammation, which would present with pale, edematous mucosa, but not black eschar. Option D involving oral antibiotics and antipyretics would not be effective against the underlying fungal infection and is not the appropriate management for invasive fungal sinusitis. Option E of observation and reassurance is not suitable for invasive fungal sinusitis as it requires prompt intervention to prevent further progression of the infection.
Image Credit:
Chae HK, Lim J, Lee SC, Kim KS. The Significance of "Black Turbinate Sign" on MRI. Ear Nose Throat J. 2020 Jul;99(6):395-396. doi: 10.1177/0145561319847628. Epub 2019 May 9. PMID: 31072199. [Link]
References:
Deutsch PG, Whittaker J, Prasad S. Invasive and Non-Invasive Fungal Rhinosinusitis-A Review and Update of the Evidence. Medicina (Kaunas). 2019 Jun 28;55(7):319. doi: 10.3390/medicina55070319. PMID: 31261788 [Article Link]
January 18th, 2023
A 58 year old male presented to the ED with a fever, facial swelling, and nasal congestion over the past two weeks. He woke up three days ago with sudden facial pain near his right eye. He reports recently being diagnosed with a condition, however he was lost to follow-up. Notable labs include an absolute neutrophil count (ANC) of 473/µL. Histopathology and CT show the following:
Which of the following is not one of the mainstays of treatment for this patient’s condition?
A. Antibacterial therapy
B. Correction of the underlying disease
C. Antifungal therapy
D. Surgical debridement
E. None of the above
-
Quiz answer: A (antibacterial therapy)
Explanation: This patient presents with acute invasive fungal rhinosinusitis (AIFR), a rare but serious disease involving fungal hyphae (as seen on histopathology of necrotic tissue) infiltrating sinus mucosa, submucosa, vasculature, and/or bone of the nasal cavity/paranasal sinuses.
Patients present with sinusitis symptoms for 4 weeks or less. CT imaging may show significant thickening of nasal and sinus mucosa, intracavity air-fluid levels, sinus opacification, middle turbinate infiltration, bony erosion, and involvement of the brain, orbit, cavernous sinus, and the pterygopalatine fossa.
Diabetes mellitus and hematologic malignancies are the most common comorbidities. The mainstays of treatment include the following: correction of the underlying disease, antifungal therapy (ie. amphotericin B, voriconazole), and surgical debridement. In this patient with neutropenia with a presumed hematologic malignancy, correction of neutropenia may require successful bone marrow transplant and the use of G-CSF (granulocyte colony stimulating factor).
References: Luo YT,https://pubmed.ncbi.nlm.nih.gov/35589479/ Zhu CR, He B, Yan AH, Wei HQ. Diagnostic and therapeutic strategies of acute invasive fungal rhinosinusitis. Asian J Surg. 2023;46(1):58-65. doi:10.1016/j.asjsur.2022.05.006
https://pubmed.ncbi.nlm.nih.gov/35589479/
November 9th, 2022
A 24-year-old patient with no significant past medical history presents in the ED with a large nosebleed, and ENT is consulted for management. On physical exam, no definitive source of bleeding can be found. Despite many attempts of applying repeated pressure, nasal packing, oxymetazoline, and cautery, the bleed is persistent and continues to be significant. Surgical intervention is planned next.
Which of the following is true about the target vessel in the next-step surgical intervention?
A. The vessel can be localized endoscopically by visualizing the lamina papyracea.
B. The vessel originates from the external carotid artery.
C. Due to the lack of branches and anastomoses from this vessel, a common complication from its ligation is tissue necrosis.
D. The vessel arises from the ophthalmic artery.
-
Quiz Answer: B
Explanation: In this patient’s case, since the bleed cannot be localized and continues to be significant, a posterior bleed is suspected. If conservative management (ie. nasal packing) fails to control bleeding, the next step is surgical intervention: usually endoscopic sphenopalatine ligation. The sphenopalatine artery (SPA) provides a majority of the blood supply to the nasal cavity and is one of the terminal branches of the internal maxillary artery, which originates from the external carotid artery. The SPA often has multiple branches and creates anastomoses with the ethmoidal arteries. Ligation of the SPA is done via endoscopic clipping or coagulation, and risk of localized hypoxia or necrosis is not common [C].
Less commonly, ligation of the anterior ethmoidal artery (AEA) or posterior ethmoidal artery (PEA) is done. Both the AEA and PEA arise from the ophthalmic artery [D]. Clipping of the anterior ethmoidal artery is considered in cases where anterior epistaxis is difficult to control. In endoscopic procedures, after maxillary antrostomy, the anterior ethmoidal cells are excavated, and the lamina papyracea is visualized. Angled lenses are then used to locate the AEA adjacent to the lamina papyracea [A].
In cases where surgical treatment fails or the patient has a high anesthetic risk, percutaneous embolization is a reasonable alternative.
References: Beck R, Sorge M, Schneider A, Dietz A. Current Approaches to Epistaxis Treatment in Primary and Secondary Care. Dtsch Arztebl Int. 2018;115(1-02):12-22. doi:10.3238/arztebl.2018.0012
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5778404/
August 24th, 2022
A 65-year-old man with a history of chronic rhinosinusitis with nasal polyposis (CRSwNP) and asthma presents to the clinic complaining of recurrent nasal obstruction, facial pain, and loss of smell despite ongoing treatment with oral corticosteroids. Over the last 10 years, he has taken oral steroids and antibiotics every 2-3 months in addition to 7 functional endoscopic sinus surgeries for recalcitrant CRSwNP. After exhausting the standard treatment options with minimal improvement, he is prescribed Dupilimab. This monoclonal antibody reduces type 2 inflammation by blocking the action of which inflammatory mediator(s):
A. IL-33
B. IL-5
C. IL-4 and IL-13
D. IgE
-
Quiz Answer: C (IL-4 and IL-13)
Explanation: Biologic therapies are an emerging treatment option for patients with poorly controlled CRS. Drugs targeting type 2 inflammatory mediators such as IL-5, IL-33, IgE and TSLP have all been developed. However, Dupilimab is the only biologic FDA approved for the treatment of poorly controlled CRSwNP. Dupilumab targets IL-4a, a shared receptor subunit between IL-4 and IL-13. Mepolizumab (anti-IL-5 monoclonal antibody), Omalizumab (anti-IgE), and Etokimab (anti-IL-33) are not currently FDA approved for the treatment of CRSwNP.
Reference: Laidlaw TM, Buchheit KM. Biologics in chronic rhinosinusitis with nasal polyposis. Ann Allergy Asthma Immunol. 2020;124(4):326-332.
May 13th, 2022
A 39-year-old female presents with nasal crusting, recurrent epistaxis, and a whistling sound coming from the nose on inspiration, all suggestive of nasal septal perforation. Which of the following would generally be the most likely cause?
A. Intranasal decongestants
B. Septal hematoma
C. Iatrogenic injury
D. Cocaine use
E. Granulomatosis with Polyangiitis
August 2nd, 2021
A 64-year-old male patient with a history of untreated hypertension presents to the emergency department with an intractable nosebleed that began a few hours ago. Over the past 3-4 days, he had nasal congestion partially relieved by over-the-counter naproxen, but has resulted in recurrent sneezing and blowing his nose frequently. He states that he also feels liquid running down his throat that tastes like metal. He initially attempted to stop the bleeding by pinching his nose and leaning forward, but his wife drove him to the ED after he began to feel dizzy and nauseous. In the ED, multiple attempts to control the bleeding with nasal packing are unsuccessful. Which of the following locations is the most likely etiology of this patient’s symptoms?
A. Anterior ethmoidal artery
B. Internal carotid artery
C. Kiesselbach plexus
D. Sphenopalatine artery
E. Superior labial artery
September 15th, 2021
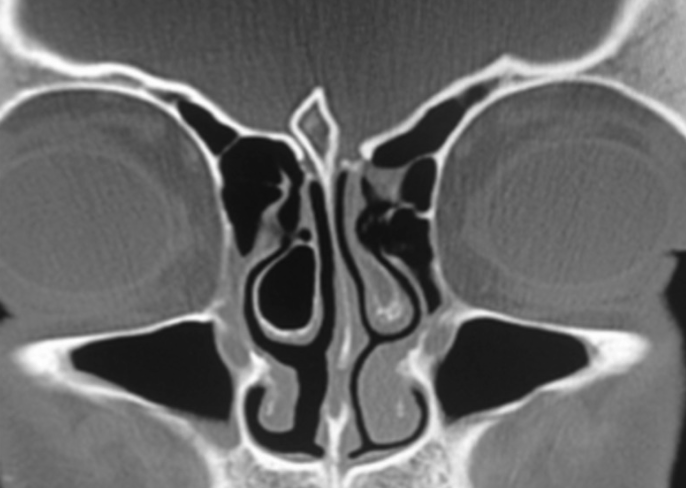
A 26-year-old male presents for a follow-up visit due to right-sided nasal discharge, obstruction, headache, and facial pain and pressure for the past 2 years, unresponsive to nasal saline, corticosteroids, antibiotics, and allergy medications. Upon review of charts, the patient is a nonsmoker and otherwise healthy without any comorbidities, including diabetes, asthma, GERD, and autoimmune diseases. His CT scan is shown below. Which of the following abnormalities is most likely causing this patient's symptoms?
A. Nasal polyp
B. Juvenile nasopharyngeal angiofibroma
C. Inverting papilloma
D. Concha bullosa
E. Meningoencephalocele
-
D (Concha Bullosa)
November 3rd, 2021
A 47-year-old female with a history of Aspirin-Exacerbated Respiratory Disease (AERD) presents to your clinic for an endoscopic sinonasal surgery evaluation. Patient was diagnosed with AERD last year, and has since been treated with multiple rounds of nasal sprays, antibiotics and low-dose systemic steroids with minimal relief. One of her CT scans is shown below:
When confirming the diagnosis of AERD, each of following could be taken into consideration EXCEPT:
A. Presence of nasal polyps on rigid endoscopy or CT scan
B. History of use of NSAIDs before the onset of asthma
C. 6-month-history of chronic rhinosinusitis
D. Watery eyes and wheezing after intranasal ketorolac
-
B (Understanding of AERD/Samter's Triad)
Samter's Triad includes the presence of bronchial asthma, nasal polyps, and aspirin intolerance. Intranasal ketorolac/oral aspirin is often used to establish the diagnosis of AERD. The history of the use of NSAIDs before the onset of asthma should not be taken into consideration, because patients develop hypersensitivity to NSAIDs AFTER the onset of asthma.